The placenta is located on the back wall overlaps the pharynx. Placenta at the edge of the internal os
The period of pregnancy is associated with future mothers with great joy and great anxiety for the health of their crumbs. These feelings are quite natural and accompany a woman for all nine months. At the same time, even if there is no reason to worry, the pregnant woman will be worried and constantly listen to her feelings. And if doctors noticed some deviations from the norm during a routine examination, it is difficult for a woman to calm down. Expectant mothers are especially frightened by the words that the placenta blocks the internal os. Many immediately begin to draw in their imagination scary pictures of what is happening to their baby, thereby further aggravating their condition.
But in fact, most pregnant women face the fact that the placenta blocks the internal os. The modern level of medicine is such that even with such a pathology, absolutely healthy and strong babies are born. However, mom must clearly understand what this diagnosis means and how to behave correctly after identifying the problem.
The placenta and its influence on the development of the child
All nine months, the mother's body provides the baby with all the necessary components for proper development. And all this happens at the expense of the placenta, which largely determines whether your baby will receive important vitamins and minerals, nutrition and oxygen, which is so important for tissues and the brain. The placenta does not form immediately in the uterus, but only towards the end of the first trimester. Previously, its role is played by the chorion - a fleecy membrane that separates the egg from the walls of the uterus. She finally matures by the twelfth day after conception. As you can see, nature very carefully made sure that the baby was constantly protected and received everything he needed.
For the normal development of the child, it is very important where exactly the placenta is attached. The chorion is usually located along the anterior wall of the uterus, posterior or near the bottom. Doctors consider the last option to be the most successful, since in this case all metabolic processes go as quickly as possible, and the baby will not experience problems getting oxygen or nutrition. However, sometimes the placenta covers the internal os completely or marginally. This is already considered a serious pathology and can cause premature birth or miscarriage. That is why doctors regularly monitor future mothers and monitor the position and maturity of the placenta by weeks. This procedure is done through ultrasound, which is quite safe for the baby and his mother. You should not refuse these studies, especially if you are over thirty-five years old. For some reason, it is in women who already have children at this age during pregnancy that the placenta blocks the internal os.
Let's talk a little about anatomy
Women often underestimate this problem and even after the diagnosis is poorly understood what exactly is happening in their body. To clarify the situation, it is necessary to turn to anatomy.
The uterus is the organ in which the baby develops for all nine months. It is connected with the vagina by the neck, which during pregnancy is tightly closed and stands out with a bluish color of the tissues. This is due to the fact that the neck becomes very dense, but at the same time elastic, because by the end of the term it will have to stretch to let the baby through. The outer and inner border of the neck is called the "pharynx". From the outside, it separates the uterus from the vagina and is tightly closed, and the internal pharynx of the cervix protects the baby from infections. At the right time, it stretches and allows the baby to take a place in the pelvis, which indicates an imminent birth.
For bearing a child, it is very important that the pharynx remains closed and does not overlap with anything, as this threatens the baby with numerous problems. The minimal ones include bleeding and increased uterine tone. In especially severe cases, the child has hypoxia of varying degrees, and the mother has difficulties with labor, forcing doctors to resort to caesarean section.

Position of the placenta
Doctors consider monitoring the position and maturity of the placenta by weeks to be very important in the process of monitoring the condition of a pregnant woman. After all, by the twelfth week it becomes possible to identify placental pathologies. Most often, women face the following two problems:
- premature maturation;
- low position relative to the pharynx.
If we talk about the first pathology, it should be noted that it is extremely rare. It can be briefly described as aging of the placenta, which does not correspond to the gestational age. That is, the baby is not yet ready to be born, and the amount of nutrients required by him is gradually decreasing. In parallel, there are problems with the provision of oxygen. All this puts the life of the crumbs in danger and forces doctors to take emergency measures.
Low placentation occurs in women quite often, but this diagnosis raises a lot of questions in pregnant women. So, what does a low placenta and a normal position of the placenta mean? Let's talk about this in more detail.
If after fertilization there was a normal attachment of the chorion (along the anterior wall of the uterus, posterior or in the bottom), then the placenta will take the desired position within the normal range. But it should be borne in mind that in nine months, as the uterus stretches, it slightly changes its position. This process is monitored by doctors during scheduled ultrasound scans. For example, if in the second trimester the distance between the internal os and the placenta is about five centimeters, then these indicators are considered normal. Around the twentieth week, the distance changes, but it should not become less than seven centimeters.
In these cases, a woman may not worry about low placentation and calmly carry the baby. If she does not have other problems, then doctors will recommend natural childbirth with a high chance of having a healthy baby.

Possible pathologies
If during an ultrasound examination the doctor noticed that the distance between the lower edge of the placenta and the internal pharynx is less than the above indicators, then we can talk about low placentation due to chorion previa. At 12 weeks, this can be noticed for the first time, then the woman will be closely monitored in order to note all possible changes in time. But in any case, we are talking about pathology.
However, I would like to note that, regardless of the stage of presentation, a woman has every chance to endure and give birth to a baby. Naturally, if you follow all the recommendations of the doctor and monitor your condition. For example, bleeding is the most likely symptom of problems caused by a low position of the placenta. Most often they occur without pain in the lower abdomen, so they do not always scare women. But any bleeding should be a reason to see a doctor, as it often indicates placental abruption, which can lead to the death of the fetus and mother.
Remember that you can talk about low chorion previa at week 12 if the distance between the placenta and the internal os is three centimeters or less. Such indicators are a cause for concern and such an entry as "pathology" is entered in the pregnant woman's card.

Presentation stages
Do not panic if the doctor tells you about the low attachment of the placenta. Not all stages of pathology are critical. Some of them require only the supervision of a doctor, while others make you think about urgent surgical intervention. Therefore, a pregnant woman herself should understand this issue.
In expectant mothers, there are three types of pathologies of the location of the placenta:
- Presentation. This stage is the most difficult, since the placenta completely covers the internal os. This pathology will not allow the baby to descend into the small pelvis and take the correct position before childbirth. Most often, the placenta on the front wall overlaps the internal pharynx, this, in addition to the already mentioned problem, can cause placental abruption. Since due to the stretching of the uterus, it will not be able to move and take the correct position. Often, the placenta on the back wall overlaps the internal pharynx, which also refers to severe pathology and threatens with problems during childbirth.
- Incomplete or partial presentation. A similar situation occurs with the marginal presentation of the chorion, in the future, the placenta is formed in the same place and its edge partially overlaps the internal pharynx. If the doctor makes such a diagnosis on ultrasound, then the woman has every chance of giving birth to the baby on her own. However, the situation must be monitored very carefully, since by the twentieth week the placenta may move. As a result, the situation of the pregnant woman will improve or, conversely, worsen.
- Low placental. If in the first days after conception, the chorion was fixed along the anterior wall of the uterus slightly lower than usual, then the placenta will form close to the internal pharynx. However, with such a diagnosis, it does not overlap with a child's place, which means that the baby has every chance of receiving the necessary nutrition and oxygen, and at the right time to be born naturally.
The stages of pathologies listed by us, doctors can only notice on ultrasound. However, before the twentieth week, the placenta may change its position, and the diagnosis will be removed. However, even in this case, a woman should carefully listen to what is happening with the baby (the 20th week of pregnancy with low placentation is decisive) in order to see a doctor in time.
Causes of presentation
As soon as a pathology is detected in a woman in a position, she begins to ask various questions. What does this mean for the baby? How to behave? At what time is a planned caesarean section done if a complete overlap of the internal os is noticed? And the main thing - what caused the pathology that arose? The last question worries expectant mothers the most, and we will try to answer it.
Doctors consider health problems to be the main reason for low placentation, which a woman could well not know about or simply not pay attention to. It is they who provoke the marginal presentation of the chorion, and then the placenta. But in a healthy future mother, the risk of such a situation is minimal. Usually, the chorion is attached along the anterior wall or posterior wall of the uterus, so in the future the distance between the edge of the placenta and the internal os will be within the normal range. During pregnancy, the doctor will monitor these indicators in order to notice problems in time. However, in most cases, if the placenta is higher than the internal os at the twelfth week, then in the control periods - twenty and thirty-two weeks - its location will be within the normal range.
But if a woman has health problems even before pregnancy, the fetal egg can attach quite low. Its location is affected by scars left after a caesarean section or abortion. Also, fibroids, adenomyosis formations and chronic inflammation of internal organs lead to a similar situation. According to doctors, any infection of the genital area can lead to pathology during pregnancy. The risk of such problems is high in cases where a woman has anatomical defects in the genital organs.

Consequences of low placentation and presentation
First of all, women should know that these problems cause fetal hypotrophy and hypoxia. This is due to malnutrition of the fetus and its supply of oxygen. In such situations, the baby signals the mother about the trouble with too high activity, so if the baby suddenly began to beat in the stomach, you should immediately consult a doctor.
Low placentation can cause placental abruption. It is always accompanied by bleeding. Obstetricians distinguish partial and complete abruption of the placenta. Partial leads to heavy bleeding at the site of detachment. A pregnant woman may not even know about the problem, but gradually her condition will worsen. Naturally, the increase in hematoma also affects the condition of the baby.
Complete abruption of the placenta is extremely dangerous. In this case, we are talking about saving the life of a little man and his mother. The problem is accompanied by severe bleeding and pain. When these symptoms appear, the count goes literally for minutes, you must immediately call an ambulance and even during the call voice your assumptions. This will facilitate the work of the arriving team of doctors, who will already have the necessary drugs prepared to save the lives of mother and baby.
If the placenta overlaps the internal os, then the woman has a chance to give birth naturally. However, to all the above listed risks, one more is added - infection with infections. Since the microflora of the vagina is not sterile, the baby can also receive a share of microbes while still in the womb. From this it is protected by a tightly closed internal pharynx. But if part of the placenta enters it, then it is likely that the infections will easily sink into the child's place. This is very dangerous for the baby.
Chances of changing the situation
Many women are interested in how to raise the placenta during pregnancy. There are stories of miracle cures and medicines that help the placenta move. However, doctors deny this rumor. They claim that so far no specialist knows how to raise the placenta. During pregnancy, numerous changes occur in a woman's body, and many of them defy any explanation, so there are cases when doctors canceled the diagnosis of "previa". But it happens naturally. Under the influence of the stretching uterus, the process of "migration" is launched. The placenta gradually begins to shift and enters the normal range. This is done very slowly and does not cause any discomfort to the pregnant woman, only at the planned ultrasound she learns that the situation has stabilized. But once again we repeat that this process does not depend on drugs.
According to statistics, in ninety-five percent of women who have been diagnosed with a pathology, the placenta has risen by the thirty-second week. For the remaining number of future mothers, the situation is also not deplorable. In about fifty percent of them, the placenta moves in the right direction by the birth.

Monitoring the condition of a woman
With low placentation, doctors may prescribe an additional ultrasound examination for a pregnant woman, but usually everything happens according to the established deadlines:
- Twelve weeks. At this time, there is a chance to notice the problem. If a woman follows the doctor's recommendations, she will not notice a deterioration in her condition. But the slightest deviation from them can cause bleeding. A pregnant woman with low placentation is strictly forbidden to get up abruptly, lift weights, play sports and have sex. It is not recommended to worry about such a problem, as well as to show emotions violently. Even joyful events can provoke minor or heavy bleeding.
- Twenty weeks. For some reason, the diagnosis may not change by the 20th week of pregnancy. What happens to the baby in this case? As the baby grows, the situation gets worse. In full presentation, there may be problems with oxygen supply and nutrition. Often a woman enters the hospital for preservation. In especially severe cases, she is left in the hospital until delivery. If a pregnant woman is diagnosed with only low placentation without overlapping the pharynx, then she may be advised to move less and monitor her condition.
- Thirty-two weeks. At this time, the situation, most likely, will not change, and doctors are thinking about how a woman will give birth. With a complete occlusion of the pharynx, we will talk about surgical intervention and the pregnant woman will be admitted to the hospital to prepare for the operation. When is a planned caesarean? If heavy bleeding does not occur, then presumably at the thirty-seventh week. In cases where it is about saving two lives, doctors make an urgent decision and can perform the operation earlier.

Dangerous symptoms and behavior algorithm
So, we think you understand that the most important symptom that needs attention, with a low placenta, is bleeding. They can be internal and external. The latter are immediately noticeable and a woman can appreciate their abundance or scarcity. Internal bleeding is not noticeable at first, but as the hematoma grows, the woman's health will deteriorate. In any case, the pregnant woman should consult a doctor, only he has the right to give recommendations and assess the patient's condition. Do not resist if he insists on the hospitalization of the expectant mother.
With low placentation, a woman must observe a special daily regimen. The health, and even the life of the baby, depends on her scrupulousness. First of all, it is necessary to exclude any physical activity. A pregnant woman should not bend over, stand up and sit down abruptly, and even more so jump and run. Failure to comply with these rules in most cases leads to detachment of the placenta.
In order for the baby not to experience problems with oxygen, walks cannot be excluded from the daily routine. They should occur regularly, as this normalizes the emotional background of the pregnant woman. It is important that a woman sleeps well. Pregnancy itself is a serious burden for the body, and with low placentation, it increases significantly. Therefore, proper sleep will help to recover and gain strength.
It is equally important to maintain a good mood and avoid stress. In the last stages, they can cause uterine hypertonicity, and this is fraught with bleeding. If they are repeated often, then a woman may experience anemia, problems with hair and nails will appear. All this will negatively affect the development of the fetus, which will also lack iron.
4790 0
Placenta previa (PP) is an incorrect attachment of the placenta in the uterus when it is located in the region of the lower uterine segment above the internal os, partially or completely overlaps it and is located below the presenting part of the fetus (i.e., in the path of the fetus being born).
Epidemiology
The frequency of PP is 0.2-0.6%.
Maternal mortality in PP ranges from 0 to 0.9%. The main cause of death is shock and bleeding. Maternal morbidity is 23%. Preterm birth occurs in 20% of cases. Perinatal mortality remains high and ranges from 17 to 26%. It is caused by prematurity and functional immaturity of the fetus, as well as its intrauterine suffering. There was no relationship between fetal death and the number of bleeding episodes during gestation, but there is a clear dependence on the amount of blood loss.
Classification
In Russia, the following classification of placenta previa is used:
■ central presentation - the internal pharynx is blocked by the placenta, the fetal membranes during vaginal examination within the pharynx are not determined;
■ lateral presentation - parts of the placenta are presented within the internal pharynx, during vaginal examination, fetal membranes, usually rough, are determined next to the placental lobules;
■ marginal presentation - the lower edge of the placenta is located at the edges of the internal pharynx, only the fetal membranes are within the pharynx;
■ low attachment of the placenta - the placental site is located in the lower segment of the uterus, but its lower edge by 7-8 cm does not reach the internal os.
■ complete placenta previa - the internal os is completely blocked by the placenta;
■ partial placenta previa - the internal os is partially blocked by the placenta;
■ marginal placenta previa -
the edge of the placenta is located at the edge of the internal pharynx;
■ low placement of the placenta - the placenta is implanted in the lower segment of the uterus, but the edge of the placenta does not reach the internal os.
Etiology and pathogenesis
The specific cause of PP is unknown. The main cause of PP is the presence of dystrophic changes in the uterine mucosa. In this case, the fertilized egg (zygote) cannot be implanted in the altered mucous membrane of the fundus and body of the uterus and descends.
Predisposing factors include inflammatory processes (chronic endometritis), a large number of births in history, abortions, post-abortion and postpartum septic diseases, uterine fibroids, deformation of the uterine cavity (scars after caesarean section and other operations, anomalies in the development of the uterus), in vitro fertilization (IVF). ) and embryo transfer, pregnancy after ovulation stimulation, drug use, advanced age of primiparas, dysfunction of the ovaries and adrenal cortex, etc.
Several theories have been proposed to explain the mechanism of PP development. According to one of them, PP occurs due to the primary implantation of a fertilized egg in the isthmus - the so-called primary isthmic placenta. The so-called secondary isthmic placenta may also occur, when it is initially formed in the body of the uterus, close to the isthmus, and then spreads to the isthmus.
Much more often it is formed from the so-called placenta capsularis. At the same time, part of the villi located in the decidua capsularis region is preserved, as a result of which not a smooth chorion is formed, but a branched one.
Clinical signs and symptoms
The clinical picture of PP before the onset of bleeding is extremely poor. There is a high standing of the presenting part of the fetus, its unstable position, often oblique or transverse position, breech presentation, often there are symptoms of threatened abortion, fetal malnutrition.
The main clinical symptom in PP is bleeding. Bleeding has its own characteristics: the absence of pain syndrome - painless bleeding, frequent recurrence and progressive anemization of the pregnant woman. Uterine bleeding in the case of PP most often occurs at a gestational age of 30-35 weeks.
Diagnosis of PP is based on clinical data. The main symptom is bleeding with red blood.
In preparation for surgery (for caesarean section), the cervix should be examined using vaginal mirrors and a vaginal examination. When viewed with the help of mirrors, bleeding from the cervical canal is detected. In a vaginal examination behind the internal pharynx, placental tissue, rough membranes are determined.
To clarify the diagnosis, ultrasound, dopplerometry, magnetic resonance imaging (MRI) are used.
Often, PP is diagnosed before the appearance of a clinical picture according to ultrasound.
Differential Diagnosis
Differential diagnosis of PP is carried out with premature detachment of a normally located placenta, rupture of the marginal sinus of the placenta, rupture of the umbilical vessels during their membrane attachment, rupture of the uterus, erosion of the cervix.
The choice of the method of therapy for PP depends on a number of circumstances, incl. on the time of bleeding (during pregnancy, in childbirth), the rate and magnitude of blood loss, the general condition of the pregnant woman (parturient woman), the condition of the birth canal (the degree of cervical dilatation), the type of PP, the duration of pregnancy, the position of the fetus, etc.
Tactics of pregnancy management
If PP is detected by ultrasound in the early stages of pregnancy and there is no blood discharge, then it is possible to observe the pregnant woman on an outpatient basis. In the presence of bleeding, treatment in a hospital is indicated. Carry out therapy aimed at removing the excitability of the uterus, strengthening the vascular wall:
Drotaverine, 2% solution, IM 2 ml 3 times a day, until the tone of the uterus normalizes and bleeding stops
Magnesium lactate / pyridoxine hydrochloride inside 2 tab. 2 r / day, until the tone of the uterus normalizes and bleeding stops
Etamzilat i / m 2 ml 2-3 r / day, until the tone of the uterus normalizes and bleeding stops.
With a gestational age of more than 16 weeks, it is possible to prescribe tocolytics:
Hexoprenaline IV drip (at a rate of 0.075-0.3 mcg / min) 0.005 mg in 500 ml of 0.9% sodium chloride solution or 500 ml of 5% dextrose solution, until uterine contractions are suppressed, then inside 0, 5 mg 4-8 r / day, several weeks or
Fenoterol IV drip (15-20 drops / min) 0.5 mg in 500 ml of 0.9% sodium chloride solution or 500 ml of 5% dextrose solution, until uterine contractions are inhibited, then inside 5 mg 4- 8 r / day, several weeks.
In preterm pregnancy, in order to prevent fetal respiratory distress syndrome, the introduction of large doses of GCS is indicated:
Dexamethasone IM 4 mg 2 times a day, 2-3 days, or orally 2 mg 4 times a day on the 1st day, then 2 mg 3 times a day for
2nd day, then 2 mg 2 r / day for 3rd day.
Tactics of labor management (choice of method of delivery)
With central, lateral and marginal PP without bleeding, delivery by caesarean section is indicated in a planned manner at a period of 37 weeks.
With severe bleeding, regardless of the degree of PP, delivery by caesarean section is indicated at any stage of pregnancy. If the placenta attaches to the anterior wall in the region of the lower uterine segment, then the corporal caesarean section is the method of choice. A transverse incision on the uterus in the lower segment can be used if the placenta is localized on the posterior wall of the uterus.
With marginal PP, expectant management can be used until the spontaneous onset of labor; in childbirth, an early opening of the fetal bladder is shown.
With low PP and in the absence of bleeding, childbirth is usually carried out through the natural birth canal.
In case of caesarean section for PP with a hemostatic purpose, the introduction of citrate-free plasma is indicated, with severe blood loss - erythrocyte mass; in addition, other hemostatic agents are used:
Aminomethylbenzoic acid IV 50-100 mg or IM 100 mg, then the dose and route of administration are selected individually according to the results of therapy
At placenta previa the internal pharynx can overlap completely and partially, depending on the type of presentation. So, with a central presentation, the internal pharynx is completely blocked, and with a lateral and marginal one and two thirds, respectively.
Regardless of the degree of throat overlap, pregnant women should adhere to the following rules:
1. Eliminate physical activity.
In order not to provoke uterine bleeding, it is recommended not to lift weights ( over 1 kg), do not run, do not make sudden movements.2. Avoid emotional stress.
A pregnant woman is advised to avoid negative emotions, worries and other conditions that can cause hypertonicity ( increased tone) and excitability of the uterus. This increases the risk of uterine contractions, which can lead to premature birth. To avoid nervous tension, it is recommended to be outdoors more often, and a pregnant woman should sleep from 8 to 10 hours a day.3. Avoid sex.
Sex is strictly contraindicated in placenta previa. Regardless of the degree of presentation, sexual intercourse should be excluded, since the placental tissue located at the uterine pharynx can be injured and, as a result, bleeding will begin.4. Mandatory hospitalization for bleeding.
At the first bleeding even insignificant) mandatory hospitalization is recommended. Further management tactics depend on the degree of blood loss and the duration of pregnancy. If the gestational age is more than 24 weeks, and the bleeding was moderate, then further hospitalization is necessary ( in the hospital) observation until the resolution of labor. Tactics of treatment depends on the accompanying complications. With hypertonicity of the uterus, drugs that lower the tone are prescribed, withThe placenta is the connection between the child and the mother, it is through it that the fetus receives nutrition and oxygen from the mother's body, giving, in turn, metabolic products.
The condition of the placenta directly determines how correctly the pregnancy will develop, and in some cases, the life of the fetus. Therefore, when placenta previa is diagnosed in a pregnant woman, doctors closely monitor her.
What is placenta previa
1. Presentation on the anterior wall. This is more likely not a diagnosis, but simply a statement of fact and it is not at all necessary that some complications will follow, although the risk of their development cannot be completely ruled out. Ideally, the placenta should be located on the back wall of the uterus, since it is in this place that the uterus is the least susceptible to changes during pregnancy.
The anterior wall is intensively stretched, thinned, which can lead to placental abruption or its further displacement to the uterine os. More about presentation on the anterior wall →
2. Lower placenta previa. Normally, the placenta is located at the bottom of the uterus. We know that the uterine fundus is on top, therefore, the pharynx is on the bottom. With a low location of the placenta (low placentation) - it is attached closer to the pharynx, not reaching it by less than 6 cm.
In this case, 2 scenarios are possible: either the placenta will drop even more, and it will be possible to talk about full or partial presentation, or it will rise up to the bottom along with the walls of the uterus increasing in size. With low placentation, as a rule, natural childbirth takes place without problems. More about lower presentation →
3. Incomplete (partial) placenta previa. There are two types of this presentation: lateral and marginal. With lateral presentation, the placenta covers the internal os (exit from the body of the uterus into the cervix) by 2/3. At the edge - by 1/3. Don't panic if you've been diagnosed with a partial presentation.
Very often, the placenta moves into its correct position before delivery. It is highly likely that childbirth is successful naturally, but everything is decided individually in each case. Learn more about partial presentation→
4. Full (central) presentation. The most severe case of abnormal location of the placenta. The placental tissue completely covers the uterine os, that is, the child simply cannot enter the birth canal. In addition, the pathology is also dangerous for the life of the mother, since the pharynx is the most extensible part of the uterus, which cannot be said about the placenta.
The uterus increases in size and there is a detachment of the placental tissue, which cannot be stretched as effectively and quickly. The integrity of the vessels is violated, which leads to severe bleeding, which, with complete placenta previa, can begin as early as the second trimester and disturb the woman until the very birth. Childbirth is only possible by caesarean section. More about full presentation →
Causes of placenta previa
The main reason is a violation of the integrity of the endometrium - the mucous layer of the uterus. A fertilized egg cannot attach itself in the most suitable place for this - at the bottom. It is there that the uterus stretches the least and can provide a high-quality metabolism between the mother and the fetus due to good blood supply.
However, due to diseases of the cardiovascular or other systems of the mother's body, fundus blood supply can be broken, and the ovum goes to look for a more suitable place for implantation.
Also, it will not be able to attach if there are scars and other endometrial damage. Usually, such deformities appear as a result of gynecological curettage, for example, during an abortion.
But the problem may not only be in the reproductive system of the mother. When underdevelopment fetal egg, it may not reach the bottom of the uterus, attaching immediately after entering it - in the area of \u200b\u200bthe internal pharynx.
Symptoms and complications
The main symptom and complication at the same time is bleeding. It is caused by placental abruption: some area of the placenta "breaks away" from the uterus, damaging the vessels. It is noteworthy that with low placentation, bleeding is internal, expressed as a hematoma. In all other cases, it is vaginal bleeding.
With partial placenta previa, bleeding begins in late pregnancy, with full - from the second trimester. In addition to the growth of the uterus itself, active physical activity, sex, gynecological examination and uterine tone can provoke bleeding.
As a result of regular, heavy bleeding, a woman may develop hypotension- stable low pressure, and anemia- low hemoglobin level. Therefore, pregnant women with presentation should be under the supervision of doctors and constantly undergo examinations. With bleeding and complete placenta previa, after 24 weeks, the woman is placed in a hospital, where she receives supportive treatment.
In some, fortunately rare, cases, placenta previa leads to fetal death.
Treatment of placenta previa
There is no medical treatment for the placenta. Doctors can not roll on this pathology. The only way out of the situation is to observe the pregnant woman, try to eliminate concomitant diseases, since any negative factor can worsen the condition, neutralize bleeding, relieve uterine tone.
Often, with placenta previa, especially central, complicated by bleeding, strict bed rest is prescribed in a hospital setting.
Childbirth with placenta previa
The main danger in childbirth is placenta previa because during contractions the placenta can completely exfoliate, and this will lead to acute fetal hypoxia, bleeding that threatens the life of the mother and the need for emergency operative delivery.
As mentioned above, natural childbirth with a low presentation is practically not a concern. With incomplete presentation - each case is considered individually. Central placenta previa is always a caesarean section at 38 weeks.

In addition, there is a possibility postpartum complications. namely the onset of bleeding. If the bleeding cannot be stopped, the uterus is removed, but these are isolated very severe cases when the life of the mother is at stake.
How to behave pregnant with placenta previa
An expectant mother diagnosed with placenta previa should protect herself from physical and emotional stress. It is necessary to exclude sudden movements, stress, overwork. Of course, this is not easy, given our rhythm of life, but the life of her child depends on it.
A woman needs good sleep, daytime rest, fresh air and emotional peace. It would be useful to revise your diet by adding iron-rich foods to it. For those who are concerned about frequent bleeding, this is a must. In addition, constipation should not be allowed. Read more about how to deal with constipation during pregnancy →
Placenta previa is a rather serious pathology that cannot but cause anxiety in the expectant mother. But she simply must pull herself together and carefully take care of herself and her baby. Moreover, today the vast majority of pregnancies complicated by presentation are easily tolerated thanks to medical care, and end in successful delivery.
Sources: http://mama66.ru/pregn/774
No comments yet!
placenta previa ( placenta praevia) - the location of the placenta in the lower segment of the uterus in the area of the internal pharynx ( prae- before and via- on a way).
The placenta can cover the internal os in whole or in part.
The frequency of placenta previa depends on the gestational age. Before 24 weeks, placenta previa is more common (up to 28%). After 24 weeks, its frequency decreases to 18% and before childbirth - to 0.2-3.0%, as the placenta moves upward ("migration of the placenta").
The degree of placenta previa is determined by the dilatation of the cervix and may change throughout labor.
During pregnancy distinguish:
Complete placenta previa, when it completely covers the internal os (Fig. 24.1, a);
Incomplete (partial) presentation, when the internal pharynx is partially blocked or the placenta reaches it with its lower edge (Fig. 24.1, b, c);
Low placenta previa, when it is located at a distance of 7 cm or less from the internal pharynx (Fig. 24.1, d).
Rice. 24.1. Variants of placenta previa. A - complete; B - lateral (incomplete, partial); B - marginal (incomplete); G - low attachment of the placenta
Placenta previa during pregnancy is determined by ultrasound. According to transvaginal echography, four degrees of placenta previa are currently distinguished (Fig. 24.2):
 Rice. 24.2. The degree of placenta previa according to ultrasound data (scheme) explanations in the text.
Rice. 24.2. The degree of placenta previa according to ultrasound data (scheme) explanations in the text.
I degree - the placenta is located in the lower segment, its edge does not reach the internal pharynx, but is located at a distance of at least 3 cm from it;
II degree - the lower edge of the placenta reaches the internal os of the cervix, but does not overlap it;
III degree - the lower edge of the placenta overlaps the internal os, moving to the opposite part of the lower segment, its location on the anterior and posterior walls of the uterus is asymmetrical;
IV degree - the placenta is symmetrically located on the anterior and posterior walls of the uterus, blocking the internal os with its central part.
For a long time, the classification of the degree of placenta previa provided for its localization during childbirth with the opening of the cervix by 4 cm or more. At the same time, they singled out:
Central placenta previa ( placenta praevia centralis) - the internal pharynx is blocked by the placenta, the fetal membranes within the pharynx are not determined (see Fig. 24.1, a);
Lateral placenta previa ( placenta praevia lateralis) - part of the placenta lies within the internal pharynx and next to it are the fetal membranes, usually rough (Fig. 24.1, b);
Marginal placenta previa ( placenta praevia marginalis) - the lower edge of the placenta is located at the edges of the internal pharynx, only the fetal membranes are located in the pharyngeal region (Fig. 24.1, c).
Currently, placenta previa, both during pregnancy and during childbirth, is diagnosed using ultrasound. This allows you to deliver a pregnant woman before bleeding. In this regard, the above classification has lost its relevance, but for an idea of the degree of placenta previa, it has a certain meaning.
In etiology placenta previa changes in the uterus and features of the trophoblast matter.
The uterine factor is associated with dystrophic changes in the uterine mucosa, as a result of which placentation conditions are violated. Chronic endometritis leads to dystrophic changes in the uterine mucosa; a significant number of births and abortions in history, especially with postpartum or postoperative endometritis; scars on the uterus after caesarean section or myomectomy, smoking.
Fetal factors contributing to placenta previa include a decrease in the proteolytic properties of the fetal egg, when its nidation in the upper sections of the uterus is impossible.
Under unfavorable conditions for nidation of the fetal egg, deviations in the development of the chorion are observed - atrophy of its villi occurs in the area decidua capsularis. At a possible location decidua capsularis a branched chorion is formed.
Due to reasons not fully known, in the early stages of pregnancy, a branched chorion is relatively often formed in the lower sections of the fetal egg. As the body of the uterus increases, the formation and stretching of the lower segment at the end of the II and III trimester, the placenta can move (migrate) up to 7-10 cm. At the time of placental displacement, small bleeding from the genital tract may occur.
With placenta previa, due to insufficient development of the uterine mucosa, a dense attachment of the placenta or its true increment is possible.
clinical picture. The main symptom of placenta previa is bleeding from the genital tract, which appears suddenly in full health, more often at the end of the II-III trimesters or with the appearance of the first contractions. With massive blood loss, hemorrhagic shock develops. The greater the degree of placenta previa, the earlier bleeding occurs. The blood flowing from the genital tract is bright scarlet. Bleeding is not accompanied by pain. It often recurs, leading to anemia in pregnant women. Against the background of anemia, relatively small blood loss can contribute to the development of hemorrhagic shock.
Bleeding is caused by detachment of the placenta from the uterine wall during the formation of the lower segment, when there is a contraction of muscle fibers in the lower sections of the uterus. Since the placenta does not have the ability to contract, as a result of displacement relative to each other of the lower segment of the uterus and the placenta, its villi are torn off from the walls of the uterus, exposing the vessels of the placental site. In this case, maternal blood flows out (Fig. 24.3). Bleeding can stop only at the end of muscle contraction, vascular thrombosis and termination of placental abruption. If uterine contractions resume, bleeding occurs again.
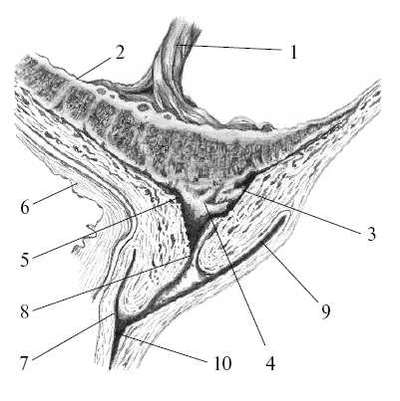 Rice. 24.3. Detachment of placenta previa.1 - umbilical cord; 2 - placenta; 3 - placental platform; 4 - detachment area; 5 - internal uterine pharynx; 6 - bladder; 7 - front arch; 8 - external uterine pharynx; 9 - posterior fornix of the vagina; 10 - vagina
Rice. 24.3. Detachment of placenta previa.1 - umbilical cord; 2 - placenta; 3 - placental platform; 4 - detachment area; 5 - internal uterine pharynx; 6 - bladder; 7 - front arch; 8 - external uterine pharynx; 9 - posterior fornix of the vagina; 10 - vagina The intensity of bleeding can be different, it depends on the number and diameter of damaged uterine vessels.
Blood from the vessels of the placental site flows through the genital tract without forming hematomas, so the uterus remains painless in all departments, its tone does not change.
With the onset of labor, one of the factors in the appearance of bleeding in placenta previa is the tension of the membranes in the lower pole of the fetal egg, which hold the edge of the placenta, and it does not follow the contraction of the lower uterine segment. The rupture of the membranes helps to eliminate their tension, the placenta moves along with the lower segment, and bleeding can stop. An additional factor in stopping bleeding with incomplete placenta previa may be its pressing by the fetal head descending into the pelvis. With complete placenta previa, a spontaneous stop of bleeding is impossible, since the placenta continues to exfoliate from the uterine wall as the cervix smoothes.
The general condition of a pregnant woman with placenta previa is determined by the amount of blood loss. It is necessary to take into account the blood that can accumulate in the vagina (up to 500 ml).
The condition of the fetus depends on the severity of anemia or hemorrhagic shock with blood loss. With heavy bleeding, acute hypoxia develops.
The course of pregnancy. When placenta previa is possible:
The threat of termination of pregnancy;
Iron-deficiency anemia;
Incorrect position and breech presentation of the fetus due to an obstacle to inserting the head to the entrance to the small pelvis;
Chronic hypoxia and fetal growth retardation as a result of placentation in the lower segment and relatively low blood flow in this part of the uterus.
Diagnostics. The main diagnostic method for both placenta previa and its variant is ultrasound. The most accurate method is transvaginal echography.
Vaginal examination with placenta previa is not recommended, as it can lead to further placental abruption, increasing bleeding. In the absence of the possibility of ultrasound, vaginal examination is carried out with extreme caution. During the study, spongy tissue is palpated between the presenting part and the fingers of the obstetrician. Vaginal examination is carried out with a deployed operating room, which allows an emergency caesarean section in case of heavy bleeding.
Management of pregnancy and childbirth with placenta previa, it is determined by the gestational age, the presence of blood discharge and their intensity.
InIItrimester pregnancy with placenta previa according to the results of ultrasound and in the absence of blood discharge, the patient is observed in the antenatal clinic. The examination algorithm does not differ from the generally accepted standard, with the exception of the additional determination of hemostasis indicators in the blood. Pregnant women are advised to exclude physical activity, travel, and sexual activity. Regularly (after 3-4 weeks) ultrasound should be performed to track the migration of the placenta.
When bleeding occurs, the woman is hospitalized. Further tactics are determined by the amount of blood loss and the localization of the placenta. With massive blood loss, a small caesarean section is performed; with minor bleeding - therapy aimed at maintaining pregnancy under the control of hemostasis. Treatment consists in the appointment of bed rest, the introduction of antispasmodics. Depending on the indicators of hemostasis, substitution (fresh frozen plasma), disaggregation (curantyl, trental) therapy or the use of drugs aimed at activating hemostasis and improving microcirculation (dicynone) is carried out. At the same time, antianemic therapy is carried out. Ultrasound control over the location of the placenta.
ATIIItrimester pregnancy with placenta previa without blood discharge, the issue of hospitalization is decided individually. If the patient lives near the maternity hospital and can get to it in 5-10 minutes, then she can be observed by the doctors of the antenatal clinic until 32-33 weeks. If the place of residence of the pregnant woman is significantly removed from the medical institution, she must be hospitalized earlier.
With abundant bleeding, urgent delivery is indicated -
abdominal and caesarean section in the lower uterine segment, regardless of the gestational age.
In the absence of blood discharge, it is possible to prolong pregnancy up to 37-38 weeks, after which, with any variant of placenta previa, in order to prevent massive bleeding, a caesarean section is performed in a planned manner. During caesarean section, especially when the placenta is located on the anterior wall of the uterus, bleeding may increase up to massive, which is caused by a violation of the contractility of the lower segment, where the placental site is located. The cause of bleeding can also be the dense attachment or accretion of the placenta, which is often observed in this pathology.
When the placenta is located on the anterior wall, an experienced doctor can perform a caesarean section in the lower segment of the uterus. In this case, it is necessary to make an incision on the uterus and placenta and continue it to the side without exfoliating the placenta from the uterine wall. Quickly remove the fetus and subsequently separate the placenta from the uterine wall by hand.
A novice doctor can perform a corporal caesarean section to reduce blood loss.
If massive bleeding occurs during caesarean section, which is not stopped after suturing the incision on the uterus and introducing uterotonic drugs, ligation of the iliac arteries is necessary. In the absence of effect, one has to resort to extirpation of the uterus.
In the presence of an angiographic installation, embolization of the uterine arteries is performed immediately after the extraction of the fetus in order to prevent massive bleeding. It is especially useful for timely ultrasound diagnosis of placental rotation during pregnancy. If this is detected on the operating table, catheterization of the uterine arteries is performed before the abdominal surgery and after the fetus is removed -
their embolization. Embolization of the uterine arteries makes it possible to perform an organ-preserving operation in case of true increment (ingrowth) of the placenta: excise part of the lower segment and suture the defect, preserving the uterus. If vascular embolization is not possible, then during ingrowth, to reduce blood loss, the uterus should be extirpated without separating the placenta.
During operative delivery, the device for intraoperative autologous blood reinfusion collects blood for subsequent reinfusion.
With incomplete placenta previa, the absence of bleeding with the onset of labor, it is possible to conduct labor through the natural birth canal, opening the membranes in a timely manner, which prevents further placental abruption. The same is facilitated by the head descending into the pelvis, which presses the exposed area of the placental site to the tissues of the uterus. As a result, the bleeding stops, and further childbirth takes place without complications. With weak contractions or with a moving head above the entrance to the pelvis after amniotomy, intravenous administration of oxytocin (5 IU per 500 ml of isotonic sodium chloride solution) is advisable. The appearance or increase in bleeding after opening the fetal bladder is an indication for operative delivery by caesarean section.
In case of incomplete presentation, absence of bleeding and premature birth, non-viable (developmental defects incompatible with life) or dead fetus after amniotomy and a movable head above the entrance to the small pelvis, it is possible to use Ivanov-Gauss skin-head forceps. In case of their ineffectiveness, a caesarean section is performed.
In the past, pedunculation of the fetus was used to stop abruption of the placenta when the cervix was not fully dilated (Brexton Hicks rotation). This complex and dangerous operation for the mother and fetus was designed for the fact that after turning the fetus on the leg, the buttocks would press the placenta against the tissues of the uterus, as a result of which the bleeding could stop.
With placenta previa in the early postoperative or postpartum period, uterine bleeding is possible due to:
Hypotension or atony of the lower uterine segment;
Partial tight attachment or ingrowth of the placenta;
Rupture of the cervix after childbirth through the natural birth canal.
To prevent violations of uterine contractility at the end of the second stage of labor or during cesarean section after the extraction of the fetus, uterotonic agents are administered: oxytocin or prostaglandin (enzaprost) intravenously for 3-4 hours.
After childbirth through the natural birth canal, the cervix must be examined in the mirrors, since placenta previa contributes to its rupture.
Regardless of the method of delivery, the presence of a neonatologist is necessary, since the fetus can be born in a state of asphyxia.
In view of the significant risk of developing purulent-inflammatory diseases in the postoperative period, the mother is shown intraoperative (after clamping the umbilical cord) prophylactic administration of broad-spectrum antibiotics to her, which is continued in the postoperative period (5-6 days).
A huge number of women face the diagnosis of "low placenta". Very often this makes them panic, looking for the causes of this condition and suitable medicines. But is the low placenta so dangerous and what is it? We need to figure it out.
After conception, the fertilized egg travels through the fallopian tubes to the uterus, where it attaches itself, where the placenta is formed. Normally, the egg is attached to the bottom of the uterus, but sometimes it falls below and is fixed on the wall or even near the pharynx itself. If the placenta is located near the cervix, we can talk about a low placenta, but if it covers the pharynx - about presentation.
Differences between a low placenta and a normal one (Video)
The placenta or the so-called child's place is a temporary organ that appears in a woman only during pregnancy. It is necessary to communicate the child's body with the mother's body and provide it with all the necessary substances. It is from the placenta that the child receives nutrients and oxygen, and decay products are excreted through it.
One of the tasks of the placenta is to prevent an immunological conflict between mother and child. At the same time, it secretes hormones necessary for both organisms.
Outwardly, the placenta looks like a disc attached to the wall of the uterus. Its diameter is about 15 centimeters, and its weight is about half a kilogram. From the side of the fetus and from the side of the uterus, the placenta is covered with special plates, between which there are many blood vessels.
The place of attachment of the placenta is of great importance. Normally, it is attached to the bottom of the uterus or next to it. In this place there are many blood vessels that create favorable conditions for the formation of optimal uteroplacental blood flow and nutrition of the embryo. But sometimes the placenta attaches below the optimal level, perhaps even in the lower segment of the uterus - this phenomenon is called a low placenta. When presenting, it is attached at the very bottom and covers the pharynx.
There are three common types of placenta previa:
- with partial presentation, the placenta partially covers the cervix of the uterus;
- with full presentation, the placenta lies across the internal os and completely covers it, separating the uterus and cervical canal;
- Cervical placentation is a rare situation when the placenta is attached in the isthmus and cervix.
The stronger the placenta overlaps the cervix, the more dangerous the situation for the mother and child.
What is the danger?
Everyone knows that a low placenta is dangerous. But what is the danger? The low placenta is, in fact, under the baby. As the pregnancy progresses, the baby grows, its weight increases, and with it the pressure on the placenta. The movements of the baby become more active, which leads to shocks on the placenta. In addition, the pressure on her is increased by too active movements of the woman. And strong pressure on the placenta can lead to bleeding.
In the bottom of the uterus, where the placenta usually attaches, there are many more blood vessels, so there are more opportunities for feeding the fetus. Incorrect attachment can threaten with a lack of oxygen and nutrients.
Very dangerous placenta previa during childbirth. In this position, a caesarean section is usually recommended to prevent premature placental abruption and severe bleeding. That is why women with a low location of the placenta in the LCD are watched especially closely. Proper management of pregnancy and childbirth, as well as the correct behavior of the woman herself, minimizes all risks.
Features of the course of pregnancy
Low attachment of the placenta can complicate the course of pregnancy, as it significantly increases the likelihood of placental abruption. During pregnancy, its lower segment grows and may increase, which is fraught with displacement of the fetus. In this case, the placenta remains in its place. This can lead to the appearance of detachment. This condition is undoubtedly dangerous, but in most cases it is not at all fatal.
It must be understood that any pregnancy requires caution and a decrease in the intensity of physical activity. A pregnancy with a low placental attachment requires doubly caution, as the likelihood of detachment and bleeding is high. When attaching the placenta at a distance of several centimeters from the internal os of the uterus, it is necessary to exclude not only strong physical exertion, but also the lifting of any objects heavier than 3-5 kg, as this can stimulate the tension of the abdominal wall. Among the forms of physical activity, leisurely walks in the fresh air can be recommended.
If the placenta blocks the internal os, the restrictions will be even greater. It is necessary to exclude not only physical work, but also sexual contacts, as well as any stress. It is important to monitor your well-being and secretions. If blood appears in them, you should immediately go to the hospital.
But you should not panic. If on a planned ultrasound at 19-20 weeks they say that there is a low attachment of the placenta without overlapping the internal pharynx, then you need to calm down and wait, following all the doctor's recommendations. In most cases, before 30-35 weeks, the placenta rises. This does not mean that she crawls over the uterus - the place of her attachment remains the same, just the uterus is stretched, and this place may be higher than it was.
Features of childbirth with low placentation and presentation
Low insertion of the placenta without occlusion of the internal uterine os is not a problem in childbirth. You can give birth naturally and there are usually no differences from other births. Problems arise if the placenta blocks the pharynx. Why is that?
Normally, during childbirth, the baby continues to feed through the umbilical cord and placenta until it comes out and begins to breathe on its own, but even after that, the connection with the placenta remains. A child comes out of the mother's womb, and the child's place still remains in the uterus. After the baby is born, the placenta comes out of the mother's body. It is no longer needed, so there is a painless and harmless process of its exfoliation.
The location of the placenta after childbirth
If the placenta is between the baby and the pharynx, then during the opening of the cervix, it can exfoliate or come off in advance, which will lead to bleeding. It turns out a situation when the child cannot exit due to the fact that the placenta blocks the exit and does not allow the cervix to open. And the opening of the CMM leads to severe bleeding, which is fraught with the death of the child and mother. Therefore, with placenta previa, a planned caesarean section is performed. With a properly performed operation, the risks for mother and child are minimal.
The most dangerous situation is cervical placentation or cervical pregnancy. Fortunately, such a pathology is extremely rare, since the only correct way to save a woman's life in this situation is to remove the uterus along with pregnancy. Any attempt to remove the fetus from the uterus leads to severe bleeding, which is too strong a threat.
Ways of prevention and treatment
Although low attachment of the placenta is called a pathology, in fact it is rather a feature. To date, doctors do not have an exact answer why the placenta is attached in the wrong place, so there can be no talk of any prevention. If the gynecologist says that the placenta is fixed lower than it should be, then there is no need to be nervous, you just need to accept this as a fact and as a guide to optimizing your lifestyle.
One of the possible reasons for improper attachment of the placenta, doctors call the presence of scars or other damage in the place of its normal localization, so it is worth treating all diseases on time and trying to avoid unnecessary surgical procedures, such as abortion.
As for treatment, there is not much to advise here either. The fact is that there are no procedures that raise the placenta, as well as drugs.. You need to understand that it is where it is. Often, pregnant women are advised to lie with their legs up - supposedly this will help the placenta rise. Now let's think about it, is it that we will hang upside down, our ears will drop? No, and the placenta will not move anywhere. The only way to raise it is to wait until the uterus grows and the place where the placenta is attached is higher than it was.
 Very often, women with a low placenta are advised to lie down "for preservation." Considering that there is no cure for this disease, the only purpose of such “preservation” is to control the woman and prevent her from harming herself. If you are sure that you can optimize your lifestyle and get to the hospital immediately when you appear, hospitalization is not necessary.
Very often, women with a low placenta are advised to lie down "for preservation." Considering that there is no cure for this disease, the only purpose of such “preservation” is to control the woman and prevent her from harming herself. If you are sure that you can optimize your lifestyle and get to the hospital immediately when you appear, hospitalization is not necessary.
Thanks
The site provides reference information for informational purposes only. Diagnosis and treatment of diseases should be carried out under the supervision of a specialist. All drugs have contraindications. Expert advice is required!
Placenta previa - definition
presentation placenta(placenta praevia - lat.) is a term used in obstetrics, which refers to various options for the location of the organ in the cervical region. This means that the placenta is located in the lower part of the uterus and overlaps the birth canal. It is the location on the way of the fetus that is born reflects the Latin designation of presentation - placenta praevia, where the word "praevia" consists of two: the first preposition "prae" and the second root "via". "Prae" means "before" and "via" means path. Thus, the literal translation of the term placenta praevia means literally "the placenta located in the way of the fetus."Placenta previa currently refers to the pathology of pregnancy, and at 37–40 weeks of gestation it occurs in 0.2–3.0% of cases. At earlier stages of pregnancy, placenta previa is noted more often (up to 5 - 10% of cases), however, as the fetus grows and develops, the uterus stretches, and its child's place moves further from the cervical region. Obstetricians call this process "migration of the placenta."
To understand the essence of the pathological location of the placenta, called previa, it is necessary to imagine the structure of the uterus, which is conventionally divided into the body, bottom and neck. The cervix is located in the lower part of the organ, and its outer part is lowered into the vagina. The upper part of the uterus, which is a horizontal platform directly opposite the cervix, is called the fundus. And the side walls located between the bottom and the cervix are called the body of the uterus.
The cervix is a kind of tightly compressed cylinder of muscle tissue with a hole inside, which is called the cervical canal. If this cylinder is stretched in width, then the cervical canal will expand significantly, forming a hole with a diameter of 9-11 cm, through which the child can exit the uterus during childbirth. Outside of childbirth, the cervix is tightly collapsed, and the opening in it is very narrow. To visualize the physiological role of the cervix, mentally draw a bag tied with a string. It is the part tied with a rope that is the very tightly compressed cervix that keeps the contents of the bag from falling out. Now turn this bag upside down so that the part tied with the string is facing the floor. In this form, the bag completely repeats the location of the parts of the uterus and reflects the role of the cervix. The uterus in the woman's stomach is located exactly like this: the bottom is at the top, and the cervix is at the bottom.
In childbirth, the cervix opens (expands) under the action of contractions, resulting in an opening through which the baby can pass. In relation to the image of the bag, the process of opening the cervix is equivalent to simply untying the rope that tightens its opening. As a result of such an "opening" of the bag, everything that is in it will fall out of it. But if you untie the opening of the bag and at the same time substitute some kind of obstacle in front of it, then the contents will remain inside, because they simply cannot fall out. In the same way, a child will not be able to be born if there is any obstacle in its path, at the site of the opening of the cervix. It is precisely such an obstacle that the placenta located in the cervical region is. And its location, which interferes with the normal course of the birth act, is called placenta previa.
With placenta previa, high neonatal mortality is recorded, which ranges from 7 to 25% of cases, depending on the technical equipment of the maternity hospital. High infant mortality in placenta previa is due to the relatively high incidence of preterm birth, fetoplacental insufficiency and abnormal position of the fetus in the uterus. In addition to high infant mortality, placenta previa can cause a terrible complication - bleeding in a woman, from which about 3% of pregnant women die. It is because of the danger of infant and maternal mortality that placenta previa is referred to as a pathology of pregnancy.
Types of placenta previa and their characteristics
Depending on the specific features of the location of the placenta in the cervical region, there are several types of presentation. Currently, there are two main classifications of placenta previa. The first is based on determining its location during pregnancy using transvaginal ultrasound (ultrasound). The second classification is based on determining the position of the placenta during labor when the cervix is dilated by 4 cm or more. It should be remembered that the degree and type of presentation may change as the uterus grows or as the cervical dilation increases.Based on the data of transvaginal ultrasound performed during pregnancy, the following types of placenta acclixity are distinguished:
1.
Full presentation;
2.
Incomplete presentation;
3.
Low presentation (low position).
Complete placenta previa
 Complete placenta previa (placenta praevia totalis - lat.). In this case, the placenta completely covers the internal opening of the cervix (internal os). This means that even if the cervix fully opens, the baby will not be able to get into the birth canal, because the placenta will block the way, completely blocking the exit from the uterus. Strictly speaking, childbirth in a natural way with full placenta previa is impossible. The only option for delivery in this situation is a caesarean section. This location of the placenta is noted in 20 - 30% of the total number of cases of presentation, and is the most dangerous and unfavorable in terms of the risk of complications, child and maternal mortality.
Complete placenta previa (placenta praevia totalis - lat.). In this case, the placenta completely covers the internal opening of the cervix (internal os). This means that even if the cervix fully opens, the baby will not be able to get into the birth canal, because the placenta will block the way, completely blocking the exit from the uterus. Strictly speaking, childbirth in a natural way with full placenta previa is impossible. The only option for delivery in this situation is a caesarean section. This location of the placenta is noted in 20 - 30% of the total number of cases of presentation, and is the most dangerous and unfavorable in terms of the risk of complications, child and maternal mortality. Incomplete (partial) placenta previa
 With incomplete (partial) presentation (placenta praevia partialis), the placenta covers the internal opening of the cervix only partially, leaving a small area free of its total diameter. Partial placenta previa can be compared to a plug that covers part of the diameter of a pipe, preventing water from moving as fast as possible. Also referred to incomplete presentation is the location of the lower part of the placenta on the very edge of the cervical opening. That is, the lowest edge of the placenta and the wall of the internal opening of the cervix are at the same level.
With incomplete (partial) presentation (placenta praevia partialis), the placenta covers the internal opening of the cervix only partially, leaving a small area free of its total diameter. Partial placenta previa can be compared to a plug that covers part of the diameter of a pipe, preventing water from moving as fast as possible. Also referred to incomplete presentation is the location of the lower part of the placenta on the very edge of the cervical opening. That is, the lowest edge of the placenta and the wall of the internal opening of the cervix are at the same level. With incomplete placenta previa in the narrow part of the lumen of the cervix, the baby's head, as a rule, cannot pass, therefore, natural childbirth in the vast majority of cases is impossible. The frequency of occurrence of this type of presentation is from 35 to 55% of cases.
Low (inferior) placenta previa
 In this situation, the placenta is located at a distance of 7 centimeters or less from the perimeter of the entrance to the cervical canal, but does not reach it. That is, the area of the internal pharynx of the cervix (the entrance to the cervical canal) with a low presentation is not captured and does not overlap with part of the placenta. Against the background of low placenta previa, natural childbirth is possible. This variant of the pathology is the most favorable in terms of the risk of complications and pregnancy.
In this situation, the placenta is located at a distance of 7 centimeters or less from the perimeter of the entrance to the cervical canal, but does not reach it. That is, the area of the internal pharynx of the cervix (the entrance to the cervical canal) with a low presentation is not captured and does not overlap with part of the placenta. Against the background of low placenta previa, natural childbirth is possible. This variant of the pathology is the most favorable in terms of the risk of complications and pregnancy. According to the results of ultrasound, in recent years, for clinical practice, obstetricians have increasingly resorted to determining not the type, but the degree of placenta previa during pregnancy, which are based on the amount of overlap of the internal opening of the cervix. Today, according to ultrasound, the following four degrees of placenta previa are distinguished:
- I degree- the placenta is located in the region of the opening of the cervix, but its edge is at least 3 cm away from the pharynx (conditionally corresponds to low placenta previa);
- II degree- the lower part of the placenta is located literally on the edge of the entrance to the cervical canal, but does not overlap it (conditionally corresponds to incomplete placenta previa);
- III degree- the lower part of the placenta blocks the entrance to the cervical canal completely. In this case, most of the placenta is located on any one wall (anterior or posterior) of the uterus, and only a small area closes the entrance to the cervical canal (conditionally corresponds to complete placenta previa);
- IV degree- the placenta is completely located on the lower segment of the uterus and blocks the entrance to the cervical canal with its central part. At the same time, identical parts of the placenta are located on the anterior and posterior walls of the uterus (conditionally corresponds to complete placenta previa).
In addition, the so-called clinical classification of placenta previa has been used for a long time, based on determining its location during childbirth when the cervix is dilated by 4 cm or more. Based on the vaginal examination during childbirth, the following types of placenta previa are distinguished:
- Central placenta previa (placenta praevia centralis);
- Lateral presentation of the placenta (placenta praevia lateralis);
- Marginal placenta previa (placenta praevia marginalis).
Central placenta previa
In this case, the entrance to the cervical canal from the side of the uterus is completely blocked by the placenta, when feeling its surface with a finger inserted into the vagina, the doctor cannot determine the fetal membranes. Natural childbirth with a central placenta previa is impossible, and the only way to bring a child into the world in such a situation is a caesarean section. Relatively speaking, the central presentation of the placenta, determined during the vaginal examination during childbirth, corresponds to the complete, as well as III or IV degree according to the results of ultrasound.Lateral placenta previa
In this case, during a vaginal examination, the doctor determines the part of the placenta that closes the entrance to the cervical canal, and the rough fetal membranes located next to it. Lateral placenta previa, determined by vaginal examination, corresponds to the results of ultrasound incomplete (partial) or II-III degree.Marginal placenta previa
 During a vaginal examination, the doctor determines only the rough membranes of the fetus protruding into the lumen of the cervical canal, and the placenta is located at the very edge of the internal pharynx. Marginal placenta previa, determined by vaginal examination, corresponds to the results of ultrasound incomplete (partial) or I-II degree.
During a vaginal examination, the doctor determines only the rough membranes of the fetus protruding into the lumen of the cervical canal, and the placenta is located at the very edge of the internal pharynx. Marginal placenta previa, determined by vaginal examination, corresponds to the results of ultrasound incomplete (partial) or I-II degree. Posterior placenta previa (placenta previa on the posterior wall)
This condition is a special case of incomplete or low presentation, in which the main part of the placenta is attached to the back wall of the uterus.Anterior placenta previa (placenta previa on the anterior wall)
This condition is also a special case of incomplete or low presentation, in which the main part of the placenta is attached to the anterior wall of the uterus. Attachment of the placenta to the anterior wall of the uterus is not a pathology, but reflects a variant of the norm.In most cases, anterior and posterior placenta previa is determined by the results of ultrasound up to 26-27 weeks of pregnancy, which can migrate within 6-10 weeks and return to its normal position by the time of delivery.
Placenta previa - causes
The placenta is formed in the part of the uterus where the fetal egg is attached. Therefore, if the egg is attached to the lower wall of the uterus, then the placenta will form in this part of the organ. The place for attachment is "chosen" by the fetal egg, and it looks for such a part of the uterus where there are the most favorable conditions for its survival (good thick endometrium, absence of neoplasms and scars, etc.). If for some reason the best endometrium ended up in the lower segment of the uterus, then the fetal egg will attach there, and subsequently this will lead to placenta previa.The reasons for the attachment of the fetal egg in the lower segment of the uterus and the subsequent formation of placenta previa are due to various factors, which, depending on the initial nature, can be divided into two large groups:
1.
Uterine factors (depending on the woman);
2.
Fetal factors (depending on the characteristics of the fetal egg).
Uterine factors- these are various pathological changes in the mucous membrane of the uterus (endometrium), formed during inflammatory diseases (endometritis, etc.) or intrauterine manipulations (abortions, diagnostic curettage, caesarean section, etc.). Fetal factors are a decrease in the activity of enzymes in the membranes of the fetal egg, which allow it to be implanted in the uterine mucosa. Due to the lack of enzyme activity, the fetal egg "slips" past the bottom and walls of the uterus and is implanted only in its lower part.
Currently, the uterine causes of placenta previa include the following conditions:
- Any surgical interventions on the uterus in the past (abortions, caesarean sections, removal of fibroids, etc.);
- Childbirth that proceeded with complications;
- Anomalies in the structure of the uterus;
- Underdevelopment of the uterus;
- Isthmic-cervical insufficiency;
- Multiple pregnancy (twins, triplets, etc.);
- Endocervicitis.
For fruitful reasons placenta previa include the following factors:
- Inflammatory diseases of the genital organs (adnexitis, salpingitis, hydrosalpinx, etc.);
- Burdened obstetric history (abortions, diagnostic curettage, difficult births in the past);
- Transferred in the past any surgical interventions on the uterus;
- Neuro-endocrine disorders of the regulation of menstrual function;
- Underdevelopment of the genital organs;
- Inflammatory diseases of the genital organs;
- uterine fibroids;
- endometriosis;
- Pathology of the cervix.
Diagnosis of placenta previa
Diagnosis of placenta previa may be based on characteristic clinical manifestations or on the results of objective studies (ultrasound and bimanual vaginal examination). Signs of placenta previa are as follows:- Bloody discharge from the genital tract of a bright scarlet color with a completely painless and relaxed uterus;
- High standing of the bottom of the uterus (the indicator is greater than that which is typical for a given period of pregnancy);
- Incorrect position of the fetus in the uterus (breech presentation of the fetus or transverse position);
- The noise of blood flow through the vessels of the placenta, clearly distinguishable by the doctor during auscultation (listening) of the lower segment of the uterus.
If it is impossible to do an ultrasound, then the doctor performs a very gentle, accurate and careful vaginal examination to confirm the diagnosis of placenta previa. With placenta previa, the gynecologist feels the spongy tissue of the placenta and rough fetal membranes with the fingertips.
If a woman does not have any clinical manifestations of placenta previa, that is, the pathology is asymptomatic, then it is detected during screening ultrasound studies, which are mandatory at 12, 20 and 30 weeks of pregnancy.
Based on the ultrasound data, the doctor decides whether it is possible to perform a vaginal examination in this woman in the future. If placenta previa is complete, then a standard two-handed gynecological examination cannot be performed, under any circumstances. With other types of presentation, you can only very carefully examine the woman through the vagina.
ultrasound diagnostics
 Ultrasound diagnosis of placenta previa is currently the most informative and safest method for detecting this pathology. Ultrasound also allows you to clarify the type of presentation (full or partial), measure the area and thickness of the placenta, determine its structure and identify areas of detachment, if any. To determine the various characteristics of the placenta, including presentation, ultrasound should be performed with moderate filling of the bladder.
Ultrasound diagnosis of placenta previa is currently the most informative and safest method for detecting this pathology. Ultrasound also allows you to clarify the type of presentation (full or partial), measure the area and thickness of the placenta, determine its structure and identify areas of detachment, if any. To determine the various characteristics of the placenta, including presentation, ultrasound should be performed with moderate filling of the bladder. If placenta previa is detected, then periodically, with an interval of 1 to 3 weeks, an ultrasound scan is performed in order to determine the rate of its migration (movement along the walls of the uterus is higher). To determine the position of the placenta and assess the possibility of conducting natural childbirth, it is recommended to perform ultrasound at the following stages of pregnancy - at 16, 24 - 25 and 34 - 36 weeks. However, if there is an opportunity and desire, then ultrasound can be done weekly.
Placenta previa - symptoms
The main symptom of placenta previa is recurrent painless bleeding from the genital tract.Bleeding with placenta previa
Bleeding with placenta previa can develop at different times of gestation - from 12 weeks to the very birth, but most often they occur in the second half of pregnancy due to the strong stretching of the walls of the uterus. With placenta previa, bleeding up to 30 weeks is observed in 30% of pregnant women, in terms of 32-35 weeks also in 30%, and in the remaining 30% of women they appear after 35 weeks or at the beginning of labor. In general, with placenta previa, bleeding during pregnancy occurs in 34% of women, and during childbirth - in 66%. During the last 3 to 4 weeks of pregnancy, when the uterus contracts especially strongly, bleeding may increase.Bleeding with placenta previa is due to its partial detachment, which occurs as the uterine wall stretches. With detachment of a small area of the placenta, its vessels are exposed, from which bright scarlet blood flows.
Various factors can provoke bleeding with placenta previa, such as excessive exercise, severe coughing, vaginal examination, sauna visits, sexual intercourse, bowel movements with strong straining, etc.
Depending on the type of placenta previa, the following types of bleeding are distinguished:
- Sudden, profuse and painless bleeding, often occurring at night, when a woman wakes up literally "in a pool of blood" is characteristic of complete placenta previa. Such bleeding may stop as suddenly as it began, or it may continue in the form of a scanty discharge.
- The onset of bleeding in the last days of pregnancy or in childbirth is characteristic of incomplete placenta previa.
Given the recurring episodes of bleeding with placenta previa, pregnant women with this pathology almost always have severe anemia, a lack of circulating blood volume (BCC) and low blood pressure (hypotension). These nonspecific signs can also be considered symptoms of placenta previa.
Also, the following signs are considered indirect symptoms of placenta previa:
- Incorrect presentation of the fetus (oblique, transverse, gluteal);
- High standing of the bottom of the uterus;
- Listening to the noise of blood in the vessels at the level of the lower segment of the uterus.
What threatens placenta previa - possible complications
 Placenta previa can threaten the development of the following complications:
Placenta previa can threaten the development of the following complications: - The threat of termination of pregnancy;
- Iron-deficiency anemia;
- Incorrect location of the fetus in the uterus (oblique or transverse);
- Breech or foot presentation of the fetus;
- Chronic fetal hypoxia;
- Delayed fetal development;
- Fetoplacental insufficiency.
Preeclampsia in placenta previa is due to the impossibility of a full-fledged second invasion of the trophoblast into the endometrium, since in the lower segment of the uterus the mucous membrane is not dense and thick enough for additional villi to penetrate into it. That is, a violation of the normal growth of the placenta during its presentation provokes preeclampsia, which, in turn, increases the severity and increases the frequency of bleeding.
Fetoplacental insufficiency is due to the fact that the blood supply to the lower segment of the uterus is relatively low compared to the fundus or body, as a result of which insufficient blood is supplied to the placenta. Poor blood flow causes an insufficient amount of oxygen and nutrients that reach the fetus and, therefore, do not satisfy its needs. Against the background of such a chronic deficiency of oxygen and nutrients, hypoxia and fetal growth retardation are formed.
Iron deficiency anemia is caused by constantly recurring periodic bleeding. Against the background of chronic blood loss in a woman, in addition to anemia, a deficiency of circulating blood volume (BCV) and coagulation factors is formed, which can lead to the development of DIC and hypovolemic shock during childbirth.
The incorrect position of the child or its breech presentation is due to the fact that in the lower part of the uterus there is not enough free space to accommodate the head, since it was occupied by the placenta.
Placenta previa - principles of treatment
 Unfortunately, there is currently no specific treatment that can change the site of attachment and location of the placenta in the uterus. Therefore, therapy for placenta previa is aimed at stopping bleeding and maintaining pregnancy as long as possible - ideally until the due date.
Unfortunately, there is currently no specific treatment that can change the site of attachment and location of the placenta in the uterus. Therefore, therapy for placenta previa is aimed at stopping bleeding and maintaining pregnancy as long as possible - ideally until the due date. With placenta previa throughout pregnancy, a woman must necessarily observe a protective regimen aimed at eliminating various factors that can provoke bleeding. This means that a woman needs to limit her physical activities, not to jump and ride on bumpy roads, not to fly in an airplane, not to have sex, to avoid stress, not to lift weights, etc. In your free time, you should lie on your back with your legs up, for example, on a wall, on a table, on the back of a sofa, etc. The position "lying on your back with your legs elevated" should be adopted at every opportunity, preferring it to just sitting on a chair, in an armchair, etc.
After 24 weeks, if the bleeding is not heavy and stops on its own, the woman should receive conservative treatment aimed at maintaining the pregnancy until 37-38 weeks. Therapy of placenta previa consists in the use of the following drugs:
- Tocolytic and antispasmodic drugs that improve the stretching of the lower segment of the uterus (for example, Ginipral, No-shpa, Papaverine, etc.);
- Iron preparations for the treatment of anemia (for example, Sorbifer Durules, Ferrum Lek, Tardiferon, Totem, etc.);
- Drugs to improve the blood supply to the fetus (Ascorutin, Curantil, Vitamin E, folic acid, Trental, etc.).
- Intramuscular injection of 20 - 25% magnesia, 10 ml;
- Magne B6 2 tablets twice a day;
- No-shpa 1 tablet three times a day;
- Partusisten 5 mg four times a day;
- Sorbifer or Tardiferon 1 tablet twice a day;
- Vitamin E and folic acid 1 tablet three times a day.
For the treatment of placental insufficiency and the prevention of fetal hypoxia, the following agents are used:
- Trental is given intravenously or taken as a tablet;
- Curantyl take 25 mg 2-3 times a day one hour before meals;
- Vitamin E take 1 tablet per day;
- Vitamin C take 0.1 - 0.3 g three times a day;
- Cocarboxylase is administered intravenously at a dose of 0.1 g in a glucose solution;
- Folic acid is taken orally at 400 mcg per day;
- Actovegin take 1 - 2 tablets per day;
- Glucose is administered intravenously.
If, during placenta previa, severe, persistent bleeding develops that cannot be stopped within a few hours, then an emergency caesarean section is performed, which is necessary to save the woman's life. In such a situation, the interests of the fetus are not thought of, since an attempt to maintain pregnancy against the background of severe bleeding during placenta previa will lead to the death of both the child and the woman. An emergency caesarean section with placenta previa is performed according to the following indications:
- Recurrent bleeding, in which the volume of blood lost is more than 200 ml;
- Regular meager blood loss against the background of severe anemia and low blood pressure;
- One-stage bleeding, in which the volume of blood lost is 250 ml or more;
- Bleeding with complete placenta previa.
Childbirth with placenta previa
With placenta previa, childbirth can be carried out both through natural routes and by caesarean section. The choice of method of delivery is determined by the condition of the woman and the fetus, the presence of bleeding, as well as the type of placenta previa.Caesarean section with placenta previa
 Caesarean section with placenta previa is currently performed in 70 - 80% of cases. Indications for caesarean section with placenta previa are the following cases:
Caesarean section with placenta previa is currently performed in 70 - 80% of cases. Indications for caesarean section with placenta previa are the following cases: 1. Complete placenta previa.
2. Incomplete placenta previa associated with breech presentation or fetal malposition, uterine scar, multiple pregnancies, polyhydramnios, narrow pelvis, primiparous age over 30, and aggravated obstetric history (abortions, curettage, miscarriages, pregnancy losses, and previous uterine surgery) );
3. Incessant bleeding with a blood loss of more than 250 ml with any type of placenta previa.
If the listed indications for caesarean section are absent, then with placenta previa, childbirth can be carried out through natural routes.
Childbirth through natural ways
Childbirth through natural routes with placenta previa can be carried out in the following cases:- Absence of bleeding or its stop after opening the fetal bladder;
- Ready for childbirth cervix;
- Regular contractions of sufficient strength;
- Head presentation of the fetus.



